Calcium and Coronary Artery Walls: Essential Knowledge for Heart Health in the 50+ Age Group
Learn how calcium impacts coronary artery health in adults over 50. Discover tips for balancing intake, preventing calcification, and maintaining overall heart health.
Introduction
Calcium is a mineral most commonly associated with bone and dental health, but many may be unaware of its role in the cardiovascular system, particularly in the walls of coronary arteries. Numerous scientific studies discuss both the benefits of calcium and the potential risks of excessive intake, especially in individuals over 50 who are at a higher risk for heart and vascular diseases.
As the body ages, calcium absorption can become less efficient. Hormonal changes and metabolic shifts also affect how calcium is processed. Understanding the balance of calcium intake and its impact on the cardiovascular system is crucial for maintaining long-term heart health. In this article, we will explore the connection between calcium and the coronary arteries, examine why calcium may accumulate in the vessel walls, and provide practical steps to prevent and manage potential cardiac issues related to calcium imbalance.
All information in this article is supported by scientific research and expert recommendations. We will also provide tips on dietary adjustments, lifestyle choices, and other best practices suited to those in their 50s and beyond who are looking to protect their hearts and reduce the risk of coronary artery disease.
What Is Calcium and Why Is It Important?
Calcium is the most abundant mineral in the human body—99% of it resides in bones and teeth, while the remaining 1% is present in the bloodstream and other tissues. This small fraction outside the skeletal system plays multiple vital roles, such as:
- Muscle Contraction: Calcium ions help trigger the contraction and relaxation of muscle fibers.
- Blood Clotting: Calcium is necessary for the coagulation cascade, preventing excessive bleeding when injuries occur.
- Nerve Signal Transmission: Calcium facilitates the movement of electrical impulses across nerve cells.
- Hormone and Enzyme Regulation: Many hormones and enzymes depend on calcium for their release and function.
Recommended Daily Intake
For adults, particularly those over 50, the daily recommended calcium intake usually ranges between 1,000–1,200 mg/day. Health professionals may recommend slightly higher amounts for individuals at risk of osteoporosis, often in combination with Vitamin D to enhance absorption.
Dietary Sources of Calcium
- Dairy Products: Milk, yogurt, cheese
- Legumes: Soybeans, black beans, chickpeas
- Dark Leafy Greens: Kale, broccoli, spinach
- Small Fish with Edible Bones: Sardines, anchovies
- Sesame Seeds: Both white and black varieties are high in calcium
While it’s important to meet the recommended intake, excessive calcium intake can lead to kidney stones and has been linked to the accumulation of calcium in arterial walls.
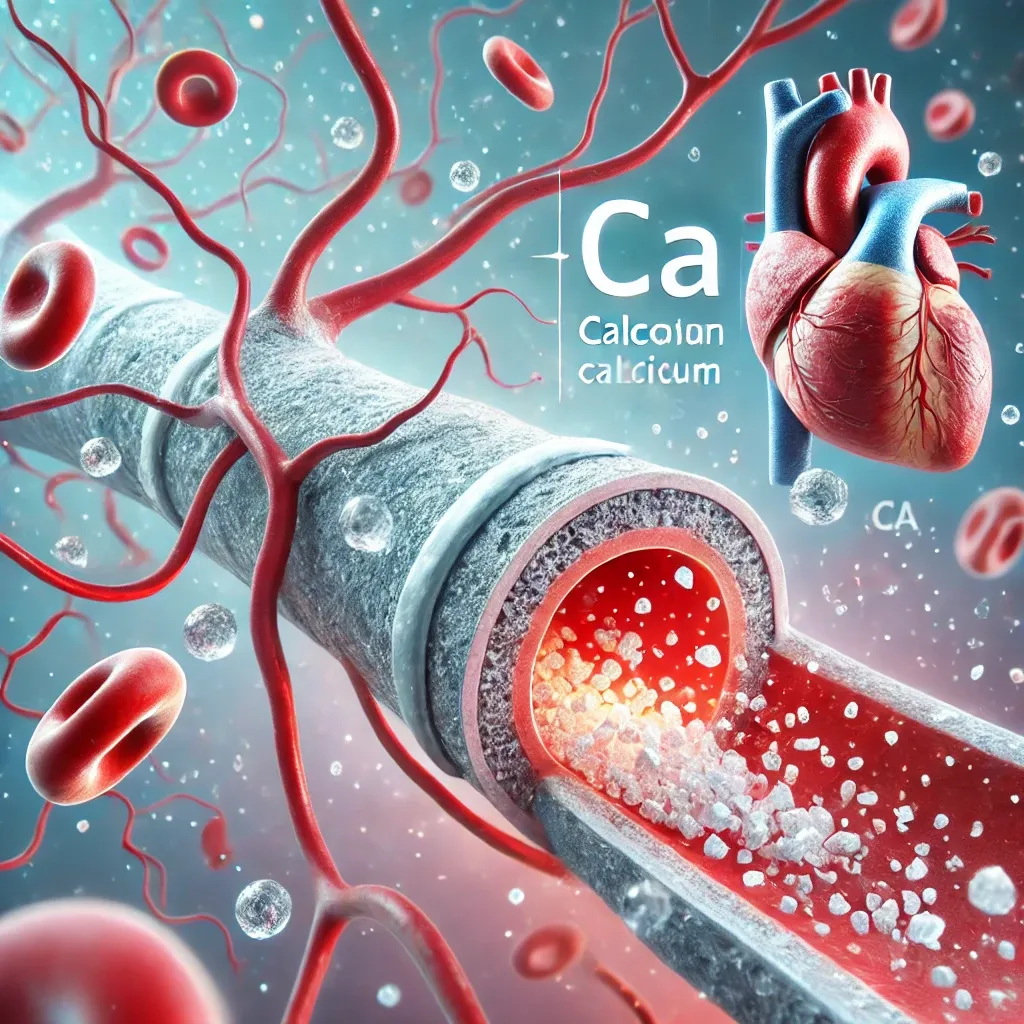
Calcium and Coronary Arteries
The coronary arteries supply blood and oxygen directly to the heart muscle. Any obstruction or calcification in these arteries can reduce blood flow, potentially leading to ischemia or even a heart attack.
Factors Leading to Calcium Accumulation
- High LDL Cholesterol (Hyperlipidemia): Oxidized LDL can build up in arterial walls, triggering inflammation and plaque formation that may incorporate calcium.
- Chronic Inflammation: Prolonged inflammation damages arteries and can accelerate calcium deposition.
- Parathyroid Gland Disorders: The parathyroid glands regulate calcium levels. Dysfunction here can cause hypercalcemia, leading to excess calcium in the blood.
- Misuse of Calcium Supplements: Taking large doses without adequate Vitamin D or Vitamin K2 may contribute to arterial calcification.
- Unhealthy Lifestyle Habits: Smoking and diets high in saturated fats or sugar exacerbate vascular damage.
Coronary Artery Calcium Score (CAC Score)
The Coronary Artery Calcium Score is a diagnostic tool that uses high-speed CT scans to detect calcium deposits in the coronary arteries. A high CAC Score generally indicates a greater risk for heart disease. Research shows that while dietary calcium is less implicated in elevating the CAC Score, calcium supplements taken in excess without proper nutritional balance may increase calcification risk.
The Risks of Excessive Calcium
- Hypercalcemia: Elevated calcium levels in the bloodstream can cause nausea, fatigue, and kidney dysfunction.
- Kidney Stones: Excess calcium can bind with oxalate or phosphate, forming stones.
- Arterial Calcification: Some studies link high supplemental calcium intake with increased plaque formation.
- Nutrient Imbalance: Too much calcium can interfere with the absorption of other minerals like iron and zinc.
Monitoring blood calcium levels and consulting healthcare providers before starting any supplements is recommended, especially for older adults or those with existing medical conditions.
Scientific Studies and Debate
There is ongoing debate regarding whether calcium significantly contributes to arterial blockage. Some studies find no strong link between dietary calcium intake and increased risk of coronary artery disease, while others suggest that high-dose calcium supplementation could promote arterial calcification.
- Journal of the American Heart Association (2016): Indicates that dietary calcium does not significantly raise coronary artery calcification risk, whereas supplements might.
- BMJ (2022): Suggests moderate calcium intake may help regulate blood pressure, but excessive intake could pose cardiovascular risks.
- Multiple Meta-Analyses: Inconclusive results due to differing dietary patterns, lifestyles, and individual risk factors.
Experts generally agree that those over 50 should consult with healthcare providers about their calcium levels, particularly if they have risk factors for heart disease.
Balancing Calcium Intake and Key Supporting Nutrients
To prevent coronary calcification, it’s important to consume calcium in combination with other nutrients:
- Vitamin D: Enhances calcium absorption from the gut and aids in bone mineralization. Found in sunlight exposure, fatty fish like salmon, and supplements.
- Vitamin K2: Directs calcium into bones and reduces arterial calcification. Present in fermented foods like natto and certain cheeses.
- Magnesium: Helps maintain balanced calcium levels and relaxes blood vessels. Sources include leafy greens, nuts, seeds, and whole grains.
- Omega-3 Fatty Acids: Reduce inflammation and support arterial health. Rich in salmon, tuna, sardines, flaxseeds, and chia seeds.
- Antioxidants: Counteract oxidative stress and chronic inflammation, which can lead to arterial damage. Found in colorful fruits and vegetables.
An overall balanced diet is crucial. Consuming high-quality proteins, healthy fats, and a variety of micronutrients can help ensure that calcium is utilized properly by the body.
Tips for Heart and Vascular Health in the 50+ Age Group
Beyond managing calcium intake, adopting a holistic approach to heart health is essential:
- Regular Exercise
- Aim for at least 150 minutes of moderate aerobic exercise (e.g., brisk walking, swimming, cycling) per week.
- Include strength training 2–3 times a week to enhance muscle and bone health.
- Balanced Diet and Weight Management
- Limit saturated fats, refined carbohydrates, and excessive sugar.
- Emphasize vegetables, fruits, whole grains, lean protein, and healthy fats.
- Limit Sodium and Sugar
- High sodium intake can elevate blood pressure and stress the heart.
- Excess sugar contributes to obesity, diabetes, and cardiovascular disease.
- Avoid Smoking and Excessive Alcohol
- Smoking damages arterial walls, increasing the risk of calcification.
- Alcohol can raise blood pressure and disturb lipid profiles.
- Regular Health Screenings
- Check cholesterol, blood glucose, and blood pressure regularly.
- Discuss advanced heart screenings like stress tests or CAC Score if risk factors are present.
- Stress Management
- Chronic stress elevates cortisol, leading to higher blood pressure and inflammation.
- Consider meditation, yoga, or other relaxation techniques.
Conclusion
Calcium is an essential mineral that benefits overall well-being, but its relationship with coronary artery walls can be a double-edged sword. In individuals over 50, it’s crucial to strike the right balance of calcium intake, combined with nutrients like Vitamin D, Vitamin K2, and magnesium. This balance can help ensure that calcium is directed into the bones rather than depositing in artery walls.
Alongside a healthy diet, maintaining a regular exercise routine, monitoring stress, and attending regular check-ups play a pivotal role in heart health. If you have a higher risk of cardiovascular disease, consulting a healthcare professional for personalized guidance on calcium supplementation and cardiac screening is a wise step.
Warnings
- The information provided in this article is for educational purposes and should not replace professional medical advice.
- If you suspect any heart-related issues, seek immediate evaluation and consultation from a qualified healthcare provider.
- Calcium supplementation should be taken under the guidance of a healthcare professional, particularly for individuals with kidney problems or parathyroid disorders.
References
- American Heart Association. (n.d.). www.heart.org
- Harvard Health Publishing, Harvard Medical School. (n.d.). www.health.harvard.edu
- Journal of the American Heart Association, 2016. “Calcium Intake From Diet and Supplement Use May Increase Coronary Artery Calcification.”
- BMJ, 2022. “Meta-analysis on Calcium and Cardiovascular Risk.”
- National Institutes of Health (NIH) – Office of Dietary Supplements. (n.d.). “Calcium: Fact Sheet for Health Professionals.”